What Makes Peritoneal Dialysis Different?
Benefits of PD
- Needle-free – You use a catheter for your treatments
- Portable – Take it with you
- Flexible – Choose treatment times that fit into your life
- Freedom – Eat and drink more of what you like and make fewer trips to the clinic
- Kidneys – PD keeps your remaining kidney function going longer than standard HD
How PD Works
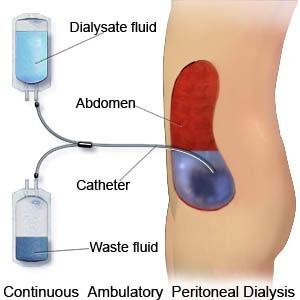
Peritoneal dialysis (PD) uses the inner lining of your belly (peritoneum) as a filter to clean your blood. A surgeon will place a soft, plastic tube (PD catheter) through the wall of your belly or chest (presternal catheter). The tube is about the size of a drinking straw. Once it heals, a nurse will teach you steps to use the tube to fill your belly with sterile fluid.
Most people use a cycler for PD—a machine that will fill your belly with the fluid and empty it out. Cycler PD is most often done at night while you sleep, so your days are free. If you can do the PD steps yourself and lift the fluid bags, you don’t need a partner for PD.
Once you put sterile PD fluid (dialysate) into your belly, it stays there, or dwells, for a few hours. While you go about your day, the fluid will collect wastes and water. Then you drain out the used fluid and put in fresh fluid. Draining and then filling is called an exchange.
Exchange Types
An exchange is when you drain out the used fluid and put in fresh fluid. There are two types of exchange;
- By Hand – Some people do four exchanges a day by hand. You might do one when you wake up, one at lunchtime, one at dinner time, and one at bedtime. Each takes about 20–30 minutes. This is called continuous ambulatory (walking around) PD, or CAPD.
- Machine – Most people who do PD use a cycler machine to do exchanges at night while they sleep. With cycler PD, your days may be free. Or, you might need to do a daytime exchange by hand, too. Your doctor can prescribe your cycler to fit your life. This is called automated PD (APD), or continuous cycling PD (CCPD).
Additional Information
Getting Ready for PD
 Your PD catheter can be placed while you are an outpatient. You won’t need to stay in the hospital overnight. Some people have little or no pain after getting a catheter; others have some pain for a few days.
Your PD catheter can be placed while you are an outpatient. You won’t need to stay in the hospital overnight. Some people have little or no pain after getting a catheter; others have some pain for a few days.
TIP 1: Ask the surgeon to put a transfer set on your catheter. This is a longer piece of tubing with a valve to open and close the catheter. Having a transfer set will help you get started with PD faster.
TIP 2: Be sure your catheter won’t exit your body at your beltline or under a skin fold. This will make it more comfortable and easy to live with and keep clean.
After surgery, your PD training nurse will check your catheter, flush it with fluid, and teach you how to change the dressings until it heals (about a week or so).
Training
Once your catheter is placed, you’ll have training. Your PD nurse will teach you how to:
- Set up a clean room to do exchanges
- Wash your hands
- Take care of your catheter and exit site
- Do an exchange
- Learn what kind of fluid to use and when to do an exchange
- Use your cycler (if you do APD or CCPD)
- Store and order your supplies
- Keep treatment logs
- Take your blood pressure
- Follow your diet and fluid limits
- Notice and report any problems
When you first start to put PD fluid into your belly, you may feel very full—even stretched. After a week or two, you’ll get used to the fluid and it won’t bother you. If feeling too full is a big problem for you, ask the nurse if you can build up slowly to the right amount over a few days.
Where to get PD
PD is the most common type of home dialysis. You can find it in all 50 states. There are more than 5,000 dialysis clinics in the U.S., and about half train people to do PD.
Space Needed
A truck will bring PD supplies to your home once a month. The driver will put the boxes where you want them. You’ll need to store 30 or so fluid boxes that are each about 1 by 2 feet, plus a couple of smaller boxes with other supplies. If you don’t have a lot of storage space, you may be able to get half of your supplies twice a month instead. You may have to miss work to be home when the supplies come.
The boxes are heavy, since they hold bags of fluid. They must stay dry. If you keep them in a basement, put them on shelves or a pallet—not on the floor. A closet is great, if you have one. Or, line up the boxes against a wall in a room where they are easy to reach. You can put a pretty sheet over them or a folding screen in front of them so you don’t have to look at the boxes.
Care Partner Tasks
In most cases, you can do PD by yourself. Even people who are blind can do PD with assist devices. If you do have someone to help, he or she may train with you. A Care Partner can gather supplies, move boxes, set up the cycler (if you use one), or in some cases, do your exchanges.
Time Requirements
You can do PD at home, at work, or when you travel. PD exchanges take about half an hour, but you can choose when to do them. Cycler PD lets you do your treatments each night while you sleep, so your days are free. Once you’re trained, you’ll only have to go to the clinic once a month to check your lab tests and treatment logs. You’ll also need time to check and order supplies each month, and then receive the shipment.